Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Paroxysmal Kinesigenic Dyskinesia Secondary to Multiple Sclerosis
*Corresponding author: Anna Planas Ballvé, MD. Department of Neurology, Complex Hospitalari Moisès Broggi, Consorci Sanitari Integral, C/Jacint Verdaguer, 90, 08970, Sant Joan Despí, Barcelona, Spain.
Received: March 24, 2022; Published: April 01, 2022
DOI: 10.34297/AJBSR.2022.16.002187
Abstract
Movement disorders, other than tremor, are uncommon during the course and initial presentation in multiple sclerosis. Among the rare movement disorders, paroxysmal dyskinesias are one of the most frequently reported. Paroxysmal dyskinesias are a group of rare movement disorders characterized by recurrent episodes of dystonia, chorea, athetosis, ballism, or a combination of these abnormal movement disorders, with normal neurologic examination between the episodes. Here we report on a patient who presented paroxysmal kinesigenic dyskinesia as the first and only clinical manifestation of multiple sclerosis that resolved completely with low doses of carbamazepine.
Keywords: Paroxysmal Kinesigenic Dyskinesia, Multiple Sclerosis
Abbreviations: PxDs : Paroxysmal Dyskinesias
PKD : Paroxysmal Kinesigenic Dyskinesia
PKND : Paroxysmal Non-Kinesigenic Dyskinesia
MS : Multiple Sclerosis
MRI : Magnetic Resonance Imaging
FLAIR : Fluid Attenuated Inversion Recovery
Introduction
Paroxysmal Dyskinesias (PxDs) are a heterogeneous group of rare conditions characterized by recurrent and brief episodes of involuntary movements that clinically can be manifested with varying combinations of dystonia, chorea and athetosis. PxDs are classified based on the precipitants of the attacks as Paroxysmal Kinesigenic Dyskinesia (PKD), Paroxysmal Non-Kinesigenic Dyskinesia (PKND) and paroxysmal exercise induced dyskinesia. Most cases of PxDs are primary, familial, or idiopathic, but they can also be secondary to other conditions such as Multiple Sclerosis (MS), vascular lesions or trauma, among others [1]. Here we report on a patient who presented PKD as the first and only clinical manifestation of MS that resolved completely with low doses of carbamazepine.
Case presentation
A 30-year-old woman was referred to our hospital due to recurrent episodes of involuntary movements on the left side of the body over a 2-month duration. The patient had no toxic habits, and her previous personal medical history was unremarkable. Her sister had epilepsy that started with febrile seizures. She explained that after a very stressful year, she presented with acute onset of recurrent brief involuntary movements, with stiffness and abnormal posture involving the left face, upper and lower left limbs. The paroxysmal events were more likely to be triggered by sudden movements, such as getting up too quickly or after a sudden acceleration from a walk to a run. These episodes only lasted up to 30 seconds and recurred more than 10 times per day. During the attack, there was no loss of consciousness or confusion. General physical and neurological examinations were normal. The patient was able to trigger an attack with specific movements such as jumping. During the attack, the patient-maintained consciousness and presented dystonic movements involving left face, hand, and feet, which lasted 30 seconds, with full recovery afterwards (Supplementary Video 1). From a phenomenological point of view, a diagnosis of PKD was made.
Laboratory workup, including complete blood count, renal and liver function tests, thyroid function, vitamins, calcium and phosphorus metabolism, folate and copper was normal. Brain Magnetic Resonance Imaging (MRI) without contrast, performed 3 months after the onset of symptoms, revealed multiple supratentorial and infratentorial white matter hyperintense T2 and Fluid Attenuated Inversion Recovery (FLAIR) lesions, being the largest in the right lateral thalamus, which showed mild restricted diffusion. Furthermore, after that initial MRI, a new cerebral and medullar MRI with contrast, that was performed 6 months after symptom onset, showed 2 new enhancing lesions in the right temporal subcortex and periventricular areas (Figure 1). Cerebrospinal fluid analysis showed oligoclonal bands. The 2017 Mc Donald diagnostic criteria for MS were fulfilled and a diagnosis of PDK as the initial manifestation of MS was made. She was treated with carbamazepine 100mg 2 times a day with complete resolution of the attacks.
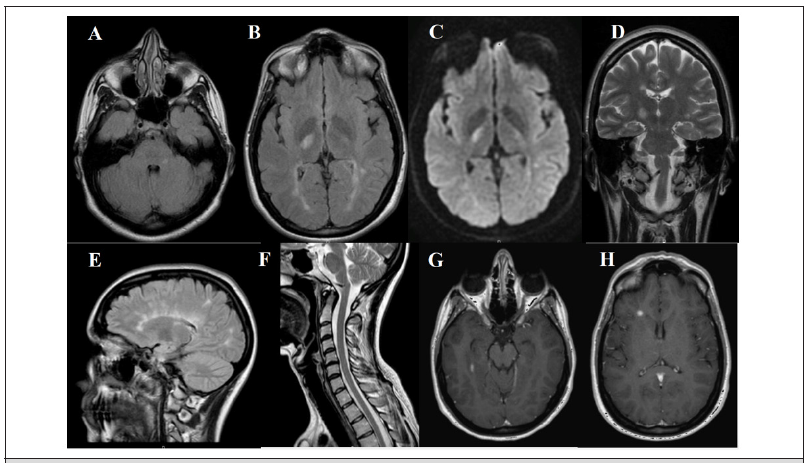
Figure 1: MRI images at three months after onset (A-D): axial FLAIR images (A, B) with supratentorial and infratentorial white matter hyperintense lesions, being the largest in the right posterior thalamus, which shows mild restricted diffusion (C); coronal T2 image (D) with hyperintense right thalamic lesion. Six months after onset (E-H): coronal FLAIR (E), T2 medullar (F) and T1 contrast images show right temporal enhancing lesion (G) and right periventricular (187
1Discussion
Other than tremor, movement disorders are traditionally thought to be uncommon in MS. Previous retrospective and review articles have estimated a prevalence of less than 2% [2,3]. However, in a recent prospective observational study, involving early MS a high prevalence of movement disorders was found with the most common in a descending order: restless legs syndrome, tremor, tonic spasms, myoclonus, focal dystonia, spontaneous clonus, fasciculations, pseudoathetosis, hyperkplexia and hemifacial spasm [4]. Even though MS has been reported to be the most common cause of secondary PxDs, there is a lack of consensus on the appropriate terminology in the literature.
Blakeley and Jankovic [1] described 76 patients with secondary PxDs with only 1 MS patient with PNKD; Ciampi et al. [5] described 7 patients with PNKD among 457 MS patients and Abboud et al. [4] report 17 patients with tonic spasms that were kinesigenic in 70%. Like our case, there are a few of other cases reported with PNKD or PKD as the initial presentation symptom of MS. Regarding neuroimaging findings, PxDs in MS have been associated with lesions throughout the central nervous system, mostly in basal ganglia and cerebellar peduncles [2]. In our patient, we think that the culprit lesion is the right posterior thalamus. Although we are not aware of the pathophysiological mechanisms, it has been proposed that is a result of transversely spreading ephaptic activation of axons. Regarding treatment, heterogeneous efficacy has been reported with methylprednisolone alone, whereas in many patients, symptomatic treatment with carbamazepine or acetazolamide is effective [5,6]. Our case, resolved completely with low doses of carbamazepine.
Conclusion
Our case illustrates that the diagnosis of PKD is essentially clinical, and it is important to consider MS in the differential diagnosis of patients presenting with PKD-like phenotype, in which lesions can be in distinct neuroanatomical regions.
Acknowledgment
Not applicable.
Conflict of Interest
The authors declare no conflict of interest.
References
- Rasmussen M (2013) Aerococci and aerococcal infections. The Journal of infection 66(6): 467-474.
- Rasmussen M (2016) Aerococcus: an increasingly acknowledged human pathogen. Clinical microbiology and infection: the official publication of the European Society of Clinical Microbiology and Infectious Diseases 22(1): 22-27.
- Lewis AL, Gilbert NM (2020) Roles of the vagina and the vaginal microbiota in urinary tract infection: evidence from clinical correlations and experimental models. GMS Infect Dis 8:
- Chang Min H, Kyeong Min J, Ji Hoon J, Yoo Jin L, Bong Soo P, et al. (2016) Urosepsis with Aerococcus urinae in a Patient with Complicated Urinary Tract Infection. Korean J Med 91(2): 229-232.
- Higgins A, Garg T (2017) Aerococcus urinae: An Emerging Cause of Urinary Tract Infection in Older Adults with Multimorbidity and Urologic Cancer. Urology case reports 13: 24-25.
- Meletis G, Chatzidimitriou D, Tsingerlioti F, Chatzopoulou F, Tzimagiorgis G (2017) An initially unidentified case of urinary tract infection due to Aerococcus urinae. The new microbiologica 40(3): 221-222.
- Skalidis T, Papaparaskevas J, Konstantinou D, Kapolou E, Falagas ME, et al. (2017) Aerococcus urinae, a cause of cystitis with malodorous urine in a child: clinical and microbiological challenges. JMM case reports 4(2): e005083.
- Schempf TBS, Beg HMD, Tenner CMD (2018) Aerococcus urinae: An under-recognized cause of UTI in internal medicine. Curr Res Integr Med 3(S1): 11-12.
- Nauka P, Durst M (2019) Septicemia from urinary tract infection with negative urinary culture: Aerococcus urinae in an older adult. Chest 156(4): A2137.
- Cai E, Pearson S, Linnebur S, Fixen D (2020) Treatment of Aerococcus Urinae in an Older Adult in Living Liver Donors. Ann Clin Case Rep 2(1): 1007.
- Otero Colón J, Farraj KL, Desai Z (2022) An Uncommon Cause of Urinary Tract Infections: A Case Report. Cureus 14(3): e23325.
- Higgins A, Garg T (2017) Aerococcus urinae: An Emerging Cause of Urinary Tract Infection in Older Adults with Multimorbidity and Urologic Cancer. Urology case reports13: 24-25.
- Sahu KK, Lal A, Mishra AK, Abraham GM (2020) Aerococcus-Related Infections and their Significance: A 9-Year Retrospective Study. Journal of microscopy and ultrastructure 9(1): 18-25.
- Yaban B, Kikhney J, Musci M, Petrich A, Schmidt J, (2020) Aerococcus urinae - A potent biofilm builder in endocarditis. PLoS One 15(4): e0231827.
- Hilt EE, Putonti, Thomas White K, Lewis AL, Visick KL, et al. (2020) Aerococcus urinae Isolated from Women with Lower Urinary Tract Symptoms: In Vitro Aggregation and Genome Analysis. Journal of bacteriology 202(13): e00170-20.
- Gilbert NM, Choi B, Du J, Collins C, Lewis A L, et al. (2021). A mouse model displays host and bacterial strain differences in Aerococcus urinae urinary tract infection. Biology open 10(8): bio058931.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.